
The Role of Nutrition in Stress Management
Can the food you eat really impact how you handle stress? While its management often focuses on mindfulness and relaxation techniques, nutrition plays a crucial but often overlooked role. Certain

Can the food you eat really impact how you handle stress? While its management often focuses on mindfulness and relaxation techniques, nutrition plays a crucial but often overlooked role. Certain
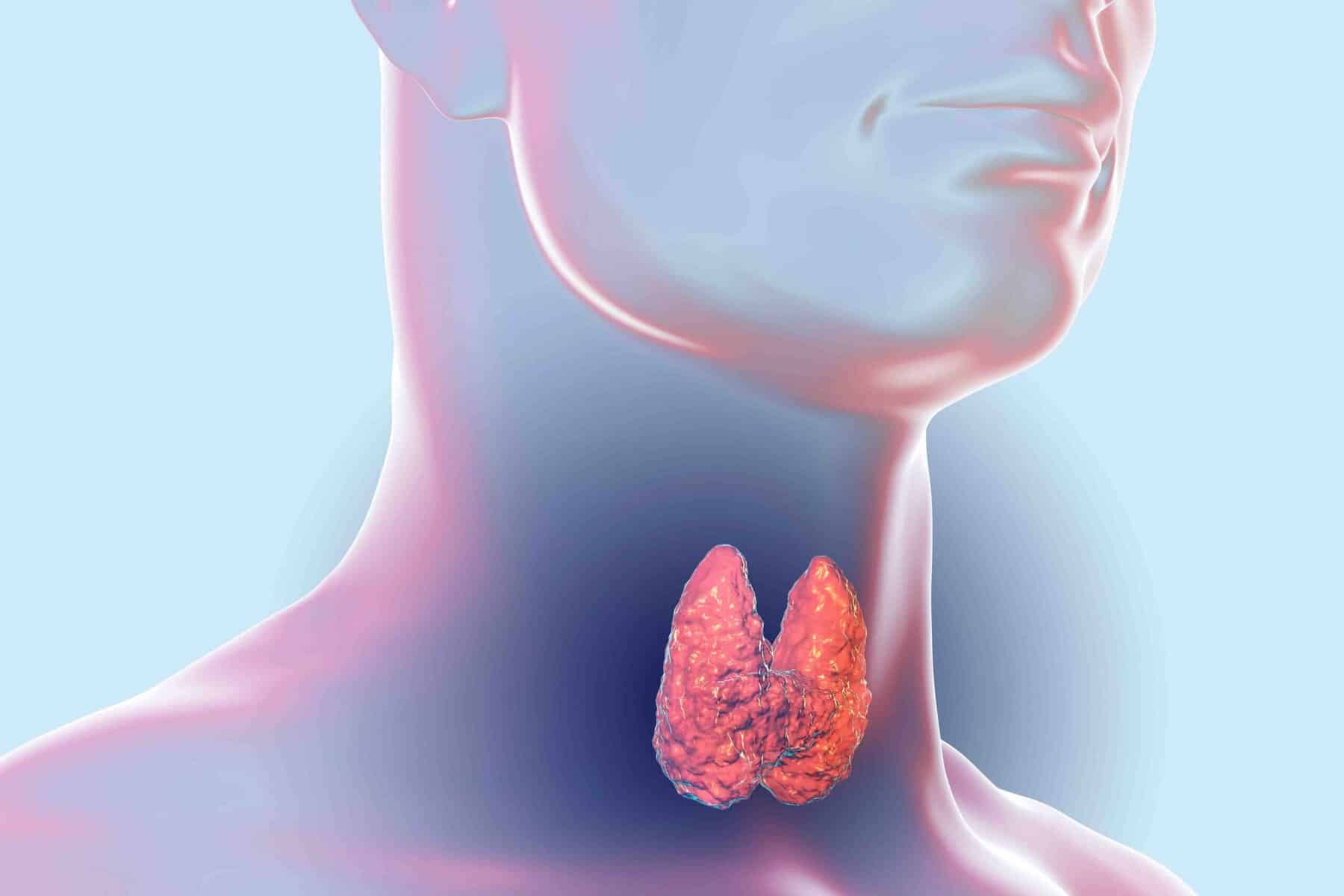
Struggling to keep weight on with hyperthyroidism? This condition speeds up metabolism, making it challenging to maintain or gain weight, no matter how much you eat. But is it really

Laser hair removal promises long-term smoothness, but how much does it really hurt? Some describe it as a mild snap, while others compare it to a rubber band sting—but is

Laser hair removal promises smooth, hair-free skin, but what about the side effects? Many people worry about redness lingering long after their sessions. Is it a temporary reaction, or could

What if the key to unlocking your body’s natural energy and vitality lies in something as simple as what you eat? The relationship between nutrition and digestive health is more

Hormones play a vital role in everything from energy levels to mood and metabolism, but did you know your diet can directly impact their balance? Eating for hormone health isn’t

Weight loss can feel like an uphill battle, especially when diet and exercise don’t seem to be enough. But could your hormones be the missing link? Hormone therapy is often

Can exercise really prevent or reverse diabetes? This question has sparked interest among experts and individuals seeking natural ways to manage their health. The connection between physical activity and blood

Struggling with mood swings, low energy, or unexplained weight changes? These could be signs of hormonal imbalances affecting your daily life. The good news is, there are natural ways to