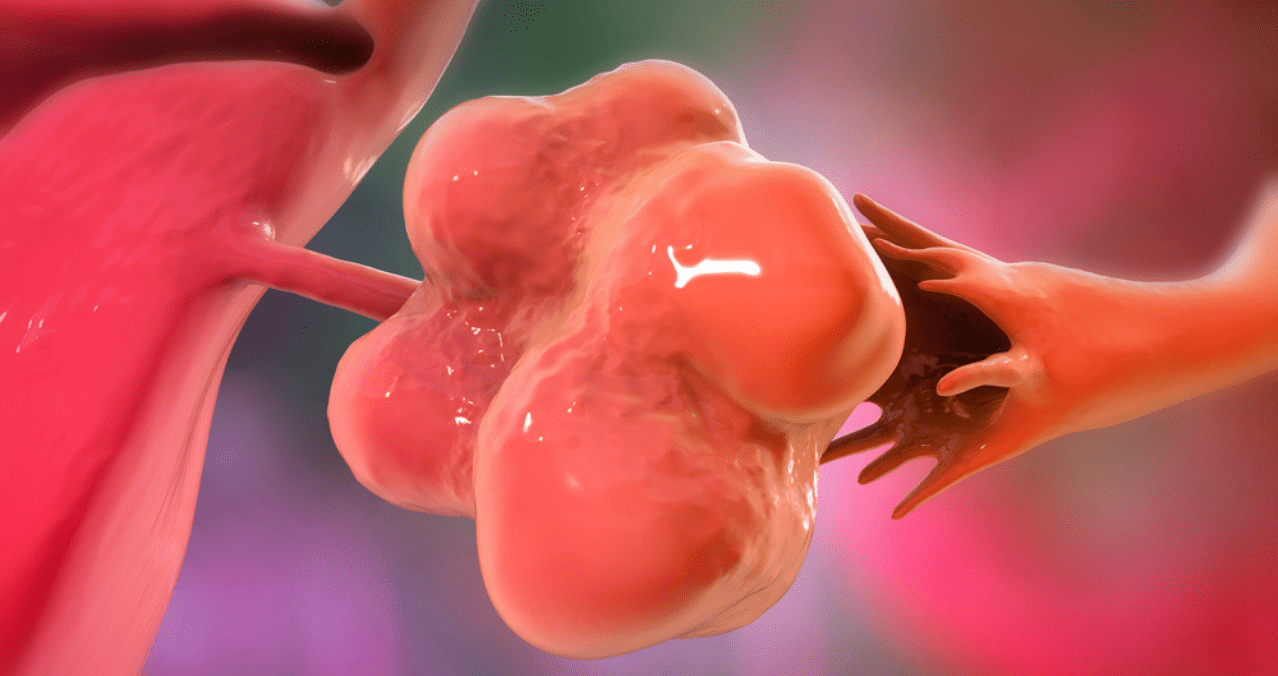
Can You Develop Polycystic Ovarian Syndrome Later in Life?
Polycystic Ovarian Syndrome is often associated with adolescence and early adulthood—but what if it could appear much later? Many women experience puzzling symptoms well beyond their reproductive peak, raising new