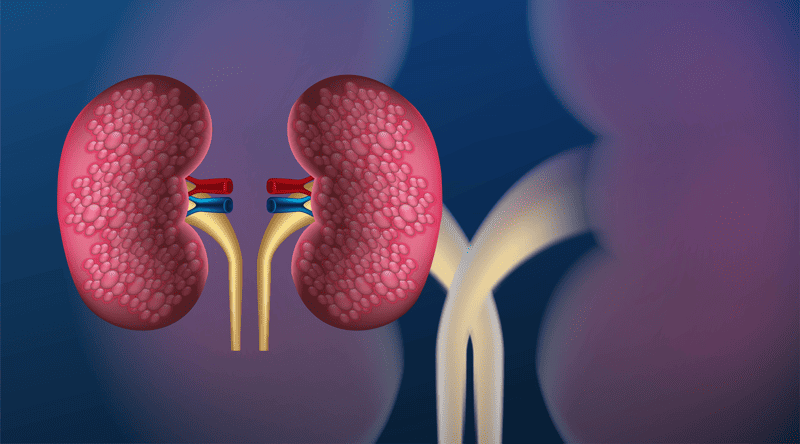
Can the adrenal glands be removed?
Have you ever wondered if it’s possible to remove the adrenal glands? This question might seem straightforward, but there’s a lot to uncover. Join us as we delve into the
Have you ever wondered if it’s possible to remove the adrenal glands? This question might seem straightforward, but there’s a lot to uncover. Join us as we delve into the

Tired of the constant battle against unwanted hair on your upper lip? Traditional methods like shaving, waxing, or threading can be time-consuming and leave behind stubble or irritation. Laser hair

When you’re facing the possibility of thyroid surgery, it’s natural to have a lot of questions. One of the biggest concerns for most people is how much it will cost,

Have you ever felt like a different person after eating a big, healthy salad compared to a greasy burger? There’s a reason for that, and it goes beyond just feeling

Have you ever wondered about the magic of laser hair removal? Imagining a life without the constant need for shaving or waxing is certainly intriguing. Let’s delve into understanding which

Imagine having a doctor who is always ready to see you, minus the long waits and hurried appointments. Sounds perfect, doesn’t it? This personalized experience is what concierge medical care
Picture this: you’re about to enter your doctor’s office, palms sweaty, mind buzzing with questions about PCOS. But what should you really be asking? As we journey through this article,
Imagine being in a vast medical maze, searching for the right doctor for diabetes. Sounds daunting, right? But, as you wander through this article, you’ll find markers guiding you straight

Weight loss surgery can be a life-changing decision for those struggling with obesity and related health problems. But with the hefty costs associated with this procedure, a common question arises: